
Osteochondrosis of the lumbar region is a pathology of the musculoskeletal system, accompanied by degenerative-dystrophic changes in bone tissue and dysfunction of the lower five vertebrae (from 20 to 24). The disease causes discomfort in the patient and is characterized by specific symptoms – pain, stiffness of movements. Osteochondrosis of the lower back occurs in waves, with periods of exacerbations and remissions. According to statistics, this form is one of the most common. Pathology left unattended often leads to irreversible changes and a significant deterioration in the quality of life. However, with a competent integrated approach, osteochondrosis can be successfully treated.
Main causes of pathology
There is no exact data on why degenerative-dystrophic changes in the spine are triggered. It is assumed that the triggering mechanism for the development of the pathology is premature age-related changes in the joints. They can be determined genetically - transmitted by inheritance, but most often they initially manifest themselves under the influence of unfavorable factors.
The main of them is considered to be poor distribution of the load on the spine. Osteochondrosis of the lumbosacral spine can develop with:
- wear high-heeled shoes;
- carry a bag or backpack on one shoulder without alternating;
- sleeping or resting for a long time in an uncomfortable position;
- sedentary work;
- lift weights.
People at risk of developing osteochondrosis include older people characterized by natural destructive changes in cartilage and bone tissue, professional athletes who train daily and intensively, pregnant women, whose center of gravity shifts asas the fetus grows and the load on the lower body shifts. the back increases significantly, office workers are forced to spend a lot of time in a sitting position.
In addition to external risk factors, doctors also call a group of internal risk factors. These include:
- previous injuries to the musculoskeletal system;
- curvature of the spine;
- flat feet;
- congenital dislocation or subluxation of the hip joint;
- autoimmune diseases;
- inflammation of joint tissues;
- pathologies of the circulatory system;
- endocrine diseases;
- obesity.
Osteochondrosis of the lower back can also be provoked by intoxication and prolonged dehydration, bad habits, calcium deficiency and any mechanical effects on the lower back - bruises, blows, falls.
Osteochondrosis of the lumbar spine: symptoms
Pathology affects not only the bone tissue itself, but also the entire movement segment of the spine: vertebrae, intervertebral discs, ligaments, surrounding soft tissues, blood vessels and nerve endings. Osteochondrosis of the lumbar spine develops, the symptoms of which become evident with significant damage, gradually and slowly. In the early stages, it is moderate discomfort during exercise, in later stages - sharp unbearable pain. Clinical signs are pronounced in the acute stage. During the remission period, they disappear, and at first this happens even without treatment.
Osteochondrosis of the lumbar spine - symptoms:
- pain in the affected area of the spine;
- irradiation of pain upward to the shoulder blade area or to the pelvis and hip joints;
- persistent feeling of tension in the lower back;
- difficulty bending and turning the body;
- slumped;
- lameness;
- muscle weakness or, conversely, increased tone;
- tingling sensation.
Not all of the symptoms described are always present at the same time. Pain may be associated with limited mobility, but not muscle weakness or numbness. Any of the signs discussed above will be a reason to consult a doctor.

Disease stages
The intensity of the symptoms that accompany osteochondrosis of the lumbosacral spine directly depends on the degree of development of the pathology. There are four in total.
- First step. The first structural and functional changes begin. The intervertebral discs dry out and can crack. At this stage, symptoms are minor. Many patients confuse them with fatigue after a day of work, wearing uncomfortable shoes, or exercising. The main signs of early osteochondrosis are mild discomfort in the lower back, which increases with bending and rotation. A slight pain is possible, which will disappear on its own after rest.
- Second step. The height of the intervertebral discs decreases, the bony structures become closer together. This causes a new set of symptoms: stiffness during movement and pain. The pain becomes prolonged and intense and may radiate to the pelvis and legs.
- Third step. At this stage, the vertebrae become deformed. Protrusions are formed - the intervertebral discs protrude into the spinal canal area, but the fibrous rings remain intact. The main symptoms are severe pain, disturbing even at rest, decreased sensitivity, crunching and clicking when moving, tingling and numbness in the lower back.
- Fourth step. Pathological changes continue to progress. The functions of the vertebrae are lost. Hernias form. Osteophytes (bony growths) form. Blood vessels may be pinched and nerve fibers pinched. Against the background of deterioration of blood circulation, the functioning of the pelvic organs is disrupted. In men, the risk of erectile dysfunction increases, in women, disturbances in the menstrual cycle are observed. Advanced osteochondrosis is manifested by acute lumbago in the lower back, lameness, reduced mobility up to complete immobility and increased temperature.
If you are worried about lumbar osteochondrosis, its treatment will directly depend on the stage at which the disease is diagnosed. In the beginning, the doctor has many more recovery methods and techniques in his arsenal. Detection of degenerative-dystrophic changes in the early stages makes it possible to treat the pathology conservatively, without resorting to surgical intervention.
Forms of pathology
The division into forms is based on the characteristics of the pain syndrome that always accompanies osteochondrosis of the sacral lumbar spine. There are three in total:
- Lumbago. This is a sharp, stabbing pain that makes it impossible to move. Causes of pain may be pinched nerves or muscle spasms.
- Lumbodynia. This is a long-term painful pain. It is characteristic of the stage of formation of protrusions and hernias. Additionally, discomfort may be associated with sprained ligaments.
- Sciatica. This is intense pain that radiates to the pelvic region. The patient complains of pain when walking, sitting, or changing body position.
Two other forms of pathology are distinguished based on the symptoms that accompany them. The patient may be diagnosed with:
- Radiculopathy. Accompanied by compression of the nerve endings due to deformation of the vertebrae. With this form of the disease, sensitivity decreases and the affected area becomes numb. Pain and tingling are felt. Possible decrease in muscle tone, impaired reflexes, tingling in the legs.
- Discogenic lumbar osteochondrosis. This is a serious illness in which the patient is limited in movement. His lower back and limbs are numb. Other symptoms are general weakness, fever, involuntary urination and, if the illness persists, weight loss.

Danger of spinal disease
If left untreated, osteochondrosis is fraught not only with unbearable pain and stiffness of movements, but also with a number of pathologies that can develop against this background. The most common complications:
- intervertebral hernia;
- inflammation of the sciatic nerve;
- radiculitis;
- paresis.
In order to prevent concomitant pathologies, it is necessary to start treatment of osteochondrosis immediately upon detection. With a competent therapeutic approach, it is possible to stop or significantly slow down the destruction of bone and cartilage tissues.
Methods for diagnosing pathology
Osteochondrosis of the sacral lumbar spine should be differentiated from other pathologies of the musculoskeletal system, which can occur with similar symptoms. The first step is a consultation with a neurologist, orthopedist or surgeon. The doctor clarifies complaints, collects anamnesis, conducts a physical examination, paying attention to the characteristics of the patient's posture and posture, the nature of his professional activity, bad habits and concomitant diseases.
For the most accurate diagnosis, instrumental techniques are used:
- MRI;
- x-ray;
- myelography with contrast material;
- Multi-cut CT.
Each of the diagnostic procedures allows the doctor to assess the current condition of the lumbar and sacral spine. The images clearly show structural changes in the vertebrae, indicating the stage of osteochondrosis. Based on the data obtained, the specialist makes a decision on the tactics of further caring for the patient.
Laboratory diagnosis is not of primary importance, however, studies may be recommended if indicated. In particular, if lumbar osteochondrosis is diagnosed, treatment may be prescribed based on the results of blood tests. They are necessary to clarify the intensity of inflammatory processes in the muscle fibers adjacent to the spine.
Lumbar osteochondrosis: treatment
The fight against pathology is carried out under the supervision of a neurologist and begins after a comprehensive diagnosis, when the degree and extent of tissue damage are determined. Modern medicine offers a number of effective conservative methods. If their use does not lead to the expected result, doctors resort to surgery.
Lumbar osteochondrosis: treatment with physiotherapy methods
All physiotherapeutic techniques are good because they affect the sacral and lumbar spine globally. This approach allows you to cope with pain, reduce inflammation and restore normal blood circulation.
When osteochondrosis of the lumbar spine progresses, treatment should be comprehensive. Patients with complaints are prescribed:
- electrophoresis - exposure of the problem area to constant electrical impulses with the possibility of using drugs for external use;
- diadynamic therapy - a variant of electrotherapy using pulsed currents;
- magnetotherapy – treatment with alternating or static magnetic fields;
- ultrasound therapy - the influence of high-frequency sound waves;
- shock wave therapy - exposure to low-frequency acoustic pulses;
It is important to consider two nuances. Firstly, the effect of physiotherapeutic treatment is noticeable only after a series of procedures, the duration of which is selected individually for each patient. The second is that physiotherapy as an independent method works for osteochondrosis of the initial degree. For large lesions, it is recommended as an auxiliary technique in addition to medical and surgical treatment.
Lumbar osteochondrosis: drug treatment
Drug therapy for lesions of the lumbar and sacral spine is aimed at relieving acute pain and suppressing inflammatory processes. The method is relevant in the acute stage, when symptoms interfere with a full life.
How to treat lumbar osteochondrosis with medication is always decided individually. A neurologist can prescribe medications belonging to different pharmacological groups. Basic:
- NSAIDs (systemic and local) to suppress inflammation of the vertebrae and adjacent tissues;
- muscle relaxants to relieve muscle spasms;
- angioprotectors to improve blood circulation;
- chondroprotectors to protect the cartilaginous tissue of the intervertebral discs from destruction;
- B vitamins to improve nerve conduction;
- painkillers for acute shooting pain that limits mobility.
Exercise therapy as a method of treating pathologies of the sacral and lumbar regions
Intense training for osteochondrosis is strictly prohibited, but you cannot completely abandon physical activity. On the contrary, exercises of moderate strength and duration help restore blood circulation and reduce pain.
How to treat osteochondrosis of the lumbar spine with exercise therapy:
- Train with an instructor. The trainer will show you which exercises are allowed in a particular situation and make sure they are performed correctly. Even the most minor technological flaws can significantly reduce the effectiveness of training and even cause damage.
- Prepare the lesson carefully. Before exercise, it is recommended to warm up the muscles - you can gently massage the lower back and sacrum.
- Strictly dose the load. The lower back is a vulnerable area. To avoid overwork, you need to monitor the duration of classes. Their optimal duration does not exceed 20 minutes.
- Gradually increase the intensity of the exercise. For beginners without experience, simple exercises and short programs are suitable. For those who have already been practicing exercise therapy for some time, you can move on to more complex options.
- Remember to be regular. One-time training will not bring visible improvements. Pain in the lumbar and sacral spine decreases if the patient regularly undergoes exercise therapy - optimally twice a week.
- Consider the contraindications. Physiotherapy has proven to be a safe method to combat osteochondrosis, but it has limitations. You should stop exercising if you feel unwell: fever, weakness, or increased temperature.
Lumbar osteochondrosis, the treatment of which should take into account the period of the disease, will not bother you if all the rules are strictly followed.
- In the acute period. Only smooth and slow movements are allowed. If the pain increases during exercise, you should stop and let your joints rest.
- In the subacute period. The pain syndrome subsides, mobility is restored, so you can slightly increase the intensity of training and increase its duration. But to avoid any deterioration, you need to carefully monitor your well-being.
- In remission. We allow the full range of exercises for pathologies of the lumbar spine, but it is important to remember that overwork leads to further exacerbation of the disease.
If lumbar osteochondrosis is diagnosed with mild or moderate severity, treatment with physical education can also take place at home. After the technique of the exercises has been perfected under the supervision of an instructor, it is not forbidden to repeat the exercises at home. To train, you will need a gymnastics mat, a roller and a ball.
Modern exercise therapy and rehabilitation rooms are equipped not only with traditional accessories, but also with special medical simulators. They help you recover from illness gently and safely, and also make activities more fun and interactive. For example, the neuromuscular rehabilitation system transforms rehabilitation into an exciting competition with oneself. The patient stands on a moving platform and performs the exercises presented on the screen. Another important advantage of the simulator is the ability to track even the slightest progress in the patient's condition. The system evaluates the result of each exercise performed and the doctor can see the progress from one workout to another. Knowing your success also motivates patients to try harder and not give up.

Manual therapy
Good results can be achieved if you supplement exercise therapy and medications for lumbar pathology with manual therapy. The method allows:
- eliminate hypertonicity of muscle fibers;
- relieve pain;
- restore blood supply to the lumbar and sacral areas;
- improve the course of metabolic processes.
Manual therapy is an effective way to correctly redistribute the load on the spine and protect yourself from further destructive changes. The advantage of this method is that it not only relieves pain, but also prevents neurological disorders that often develop against the background of lumbar osteochondrosis.
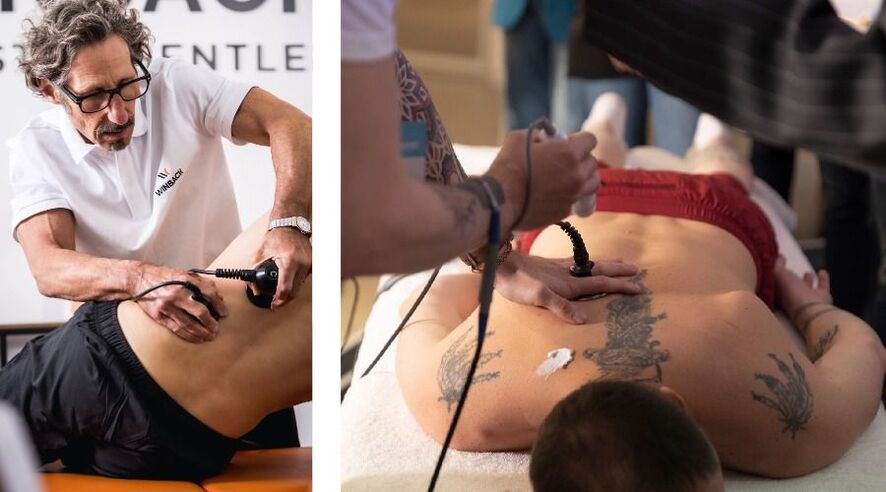
Currently, chiropractors combine massage and physiotherapy methods, such as tecartherapy. Electromagnetic waves penetrate deep into bone tissue and help relieve pain attacks and quickly restore mobility.
Surgical methods
Osteochondrosis of the lumbar spine, drug treatment of which, physiotherapy and exercise therapy is not always effective, significantly complicates the patient's life. In some cases, only surgical intervention is applicable to eliminate pain and restore back mobility. Modern methods and technological equipment make it possible to perform minimally invasive operations with a shortened rehabilitation period.
For osteochondrosis, the following methods of intervention are relevant:
- endoscopic excision of intervertebral hernia – using microsurgical instruments and a built-in camera;
- transfacet ablation of intervertebral hernia – using neurosurgical tube dilators;
- laminectomy – surgical removal of pathologically altered bony processes;
- microdiscectomy – removal of hernial protrusion.
Direct indications for surgical intervention are recurrent hernias, spinal stenosis, when the spinal canal narrows, and degenerative spondylolisthesis, a pathology in which the vertebrae are displaced relative to each other. In all other cases, if osteochondrosis of the lumbar spine is confirmed, doctors try to carry out treatment using conservative methods.
Disease prevention
The symptoms of osteochondrosis cause inconvenience, and treatment of the pathology can take a long time. It is much more effective to protect the vulnerable lumbar region from overstrain in advance. As a preventative measure, it is recommended:
- Organize your workplace properly during office work. The back of the chair should support the lower back and the table should be adjusted to the height.
- Avoid uncomfortable shoes. The optimal heel height for women is up to 5 cm. It is also advisable to exclude flat insoles, as they contribute to foot deformation and flat feet - one of the factors.
- risk of osteochondrosis.
- Exercise. You should avoid lifting heavy objects. Swimming, walking and cardio training are useful if there are no contraindications.
- Eat a balanced diet. The diet should contain foods that are sources of calcium, phosphorus and B vitamins. These include fish, dairy products, leafy vegetables and cereals. These substances are necessary to strengthen all elements of the joints and support the nervous system.
- Make sure you get enough sleep. It is best to sleep on an orthopedic mattress of medium hardness. It will provide an anatomically correct posture in which the body will rest from daily stress.
- Control body weight. Obesity is one of the provoking factors. If the weight is normal, the load on the spine will be adequately distributed and the risk of circulatory disorders will be minimized.
The prognosis of patients with osteochondrosis directly depends on the degree of damage to the vertebrae. This is why rapid diagnosis is extremely important. If you are concerned about lower back pain and the pictures reveal destructive processes in the early stages, you should start treatment. In the early stages, medications and physiotherapy are effective. In later cases, it is rarely possible to do without surgical intervention. Exercise therapy can be used as an additional measure of assistance in any form and at any stage.






























